The rise in data analytics, electronic health records and an increased focus on patient-centricity is driving change in clinical trial operations. As a result, the relationships between stakeholders within the clinical trial ecosystem is changing too.
Key within this paradigm shift is a move towards greater collaboration and data sharing. In this post, we explore what these changes look like and how stakeholders need to connect with each other.
Data Collection Impacts Relationships
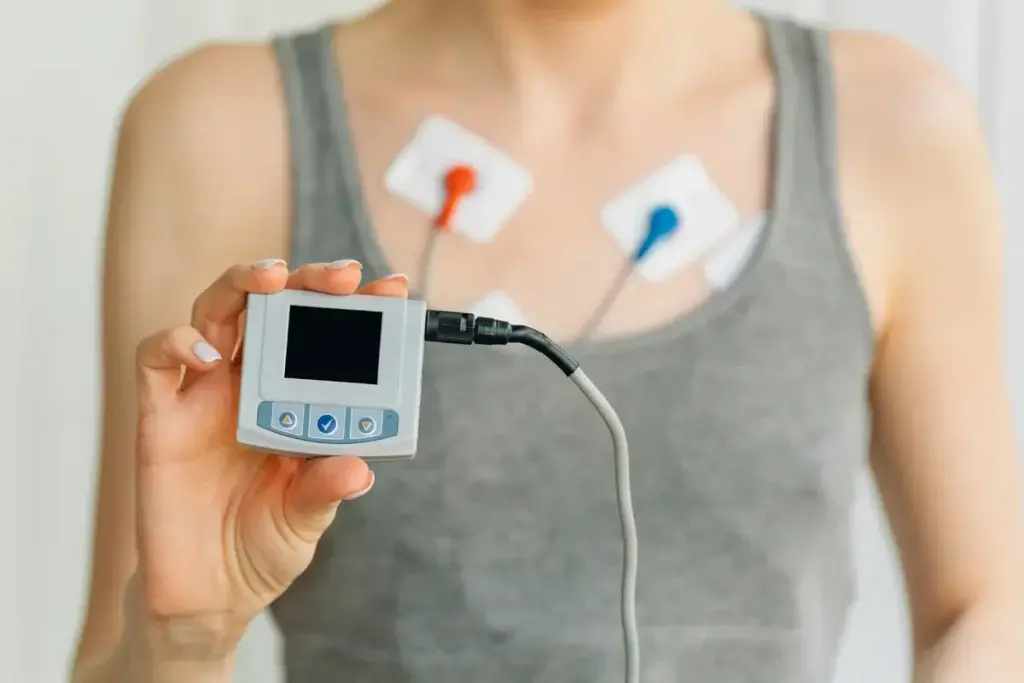
Clinical trials require subjective data from patients but this has not always been easy. With IoT sensors and wearables, however, researchers now have better access to more and better quality real-world data, such as patients’ heart rates, glucose levels and blood pressure numbers.
This type of data means improved relationships within the contract research organizations, site staff and patients ecosystem. The patient experience is better too. There’s no longer need to manually fill in personal data reports plus less travel to sites is required, says tech futurist Richard van Hooijdonk. The result is fewer patients dropping out, better trial outcomes and further advancement of research.
Data Sharing Becomes Essential
The goal of interoperable, shareable data across the industry will result in far more efficient clinical research and greater collaboration between multiple trial stakeholders.
And while this is far from the norm at present, the Oncology Clinical Trial Information Commons is one example of a platform making this collaborative relationship a reality, writes Martin Naley, consultant at Thrive Earlier Detection.
The platform holds clinical trial data. Pharma companies can use the platform to update trial data and other parties can mine data in a consistent and machine-readable format. This includes patient selection criteria in order to match patient eligibility, trial locations and patient participation requirements.
The platform will also grant access to government registry programs, patient advocacy organizations, health institutions and technology developers, resulting in a thriving ecosystem. Data will be able to be set to proprietary and shareable categories. Nine founding member organizations have joined forces to make clinical trial information available, sharing current technologies and approaches, with a view to making the entire oncology clinical trial ecosystem more efficient.
Patient-Facing Technologies
Patient-facing technology (PT) puts patients first by being responsive to their particular needs. It also improves data collection. Further, these technologies are desirable within the perspective of a clinical trial ecosystem, writes Matthew Moyer, director of clinical supply technology at Merck.
Site staff regard the use of PT favorably according to surveys, with 28.5 percent saying patient-facing tech increased their desire to participate as a site. More than 60 percent of respondents agree that sites are willing to use PT in clinical research. Yet accessing the right technological support inhibits the uptake of PT. And sites says that sponsors need a better understanding of PT’s value too.
Interestingly, sites consider PT a potential burden to patients, while sponsors believe it will enhance the patient experience. Patients, on the other hand, are pragmatic. They understand trials need to be treated on an individual basis and technology should improve the experience but not replace all in-person trial interactions. Nevertheless stakeholders appreciate that PT requires a collaborative approach to ensure everyone understands why it’s being used and how to use it.
When it comes to any technology used to gather data, simplicity is key, say ICON’s Marie McCarthy and Chen Admati at Intel. This simplicity, however, requires experienced study teams put into place a digital framework that is tried and tested and supports full integration of systems and processes.
The Arrival of Integrated Research Organizations
The goal for clinical research is easier collaboration and improved relationships among stakeholders. This is why the team at clinical research services provider Javara believe an integrated research organization (IRO) is the answer.
The core tenet is alignment of stakeholder goals within the clinical trial ecosystem. For instance, an IRO would align clinical trials with population health initiatives at a healthcare organization or integrate clinical trials as a care option. Alignment might also concern increasing patient protection through improved data security and using evidence-based predictions of a trial’s performance.
Indeed, the Javara team consider integration of research into routine healthcare as the pressing need of the industry. Within this approach, collaboration, data sharing and the continued mindfulness of patient-centricity will shape stakeholder relationships.
This journey towards integration has another effect: The need and desirability for specialized roles will decrease. The team at Veradigm suggest thinking about trial staff as a network of research clinicians empowered and connected by technology. From this perspective, electronic health records become essential to the new ecosystem as do interoperable systems and data sharing.
Prevention Rather Than Cure
The clinical research ecosystem is evolving through a shift in focus. Patients and payers understand that it’s better and more cost-effective to slow the progression of a condition or to prevent it altogether rather than treating it after it materializes, explain Fritz Heese and Julian Offenhammer at management consulting firm Oliver Wyman.
The result is new players in the clinical research ecosystem. Heese and Offenhammer refer to condition management innovators that employ tech and data analytics to monitor and engage patients to modify problematic behaviors. The goal is mitigation and management of conditions through a proactive approach to treatment.
Consequently, pharma has seen the value in partnering with these innovators. Sanofi, for example, has partnered with condition health company Omada, and Roche has acquired Flatiron Health, an oncology data company, writes Heese and Offenhammer.
Another example of this shift towards promoting wellness rather than treating illness is Cityblock, which gives community healthcare practitioners structured and unstructured data to create personalized wellness plans to encourage healthy behavior in people living in neighborhoods with high poverty rates and other social challenges.

Relationships Between Sponsors and Trial Sites
Selecting the right site is an important choice that can result in the success or failure of clinical research. Sites with proven track records — especially in the research area in question — can improve recruitment and retention rates and adhere to the necessary protocol. Automation technology has delivered greater consistency into the site selection and validation processes, explains Denise Myshko at PharmaVoice.
Myshko refers to Merck’s use of automation of site selection through WCG’s Site Feasibility Solution. Based on therapeutic and enrollment trends, the result for Merck is a narrowed and more relevant group of investigators and trial sites. The gain from this approach is obvious: Partnerships between sponsors and sites will be more advantageous and mutually beneficial as they will be better aligned from the very beginning.
CROs and Sponsors as Partners
The relationship between sponsors and contract research organizations has changed for the better. Indeed, as pharma companies outsource more services, they appreciate the strategic value CROs can bring. The result is a partnership rather than client-vendor relationship between the two, writes Krista Armstrong, SVP of clinical development services and head of neurosciences at Premier Research.
CROs have also been driving the shift in the relationship. They’ve understood that successful research requires collaboration over transaction. And CROs demonstrated how pharma can benefit from their help with planning, protocol, budgeting, compliance and more.
Pharmaceutical Physicians Must Engage Patients
The role of pharmaceutical physicians — doctors working for pharma companies — has broadened to fulfill a medical affairs function. These doctors are tasked with extending medical engagement activities to patient associations, according to research published in Advances in Medical Education and Practice.
Engaging patients and patient associations aims to gather patient insights, define meaningful endpoints and improve treatment. It also follows the directive of the FDA to include patients in drug development as early as possible.
Hospitals and Pharma Manufacturers
Hospitals used to be simple purchasers of products from pharma manufacturers but the relationship is changing. Michael J. Dowling, president and CEO at Northwell Health, says independent hospitals are now part of a broader healthcare ecosystem and traditional models of purchasing no longer work due to new policies governing them.
Rather than pharma sales reps marketing to the 40 percent of US physicians working for hospitals or large integrated health systems, Dowling says an enterprise partnership is preferable. This takes the transactional relationship further to include collaboration on clinical trials and research. Pharma needs to sell the drugs and hospitals need to buy them, but working together can cut costs and improve quality and efficiency.
The way clinical trials operate is constantly changing. New technology, streamlined processes and an abundance of data are some of the key drivers of this change. Stakeholders in the evolving clinical trial ecosystem can adapt by enhancing the way they interact, choosing greater collaboration and transparency.
